Two Researchers From CHS Receive K-awards from NIH
By Ryan Clark
CHS Communications Director
Two young investigators from the College of Health Sciences have recently received highly competitive K-award funding from the National Institutes of Health for their research, reports Esther Dupont-Versteegden, PhD and professor in Physical Therapy, as well as Director for the Center for Muscle Biology.
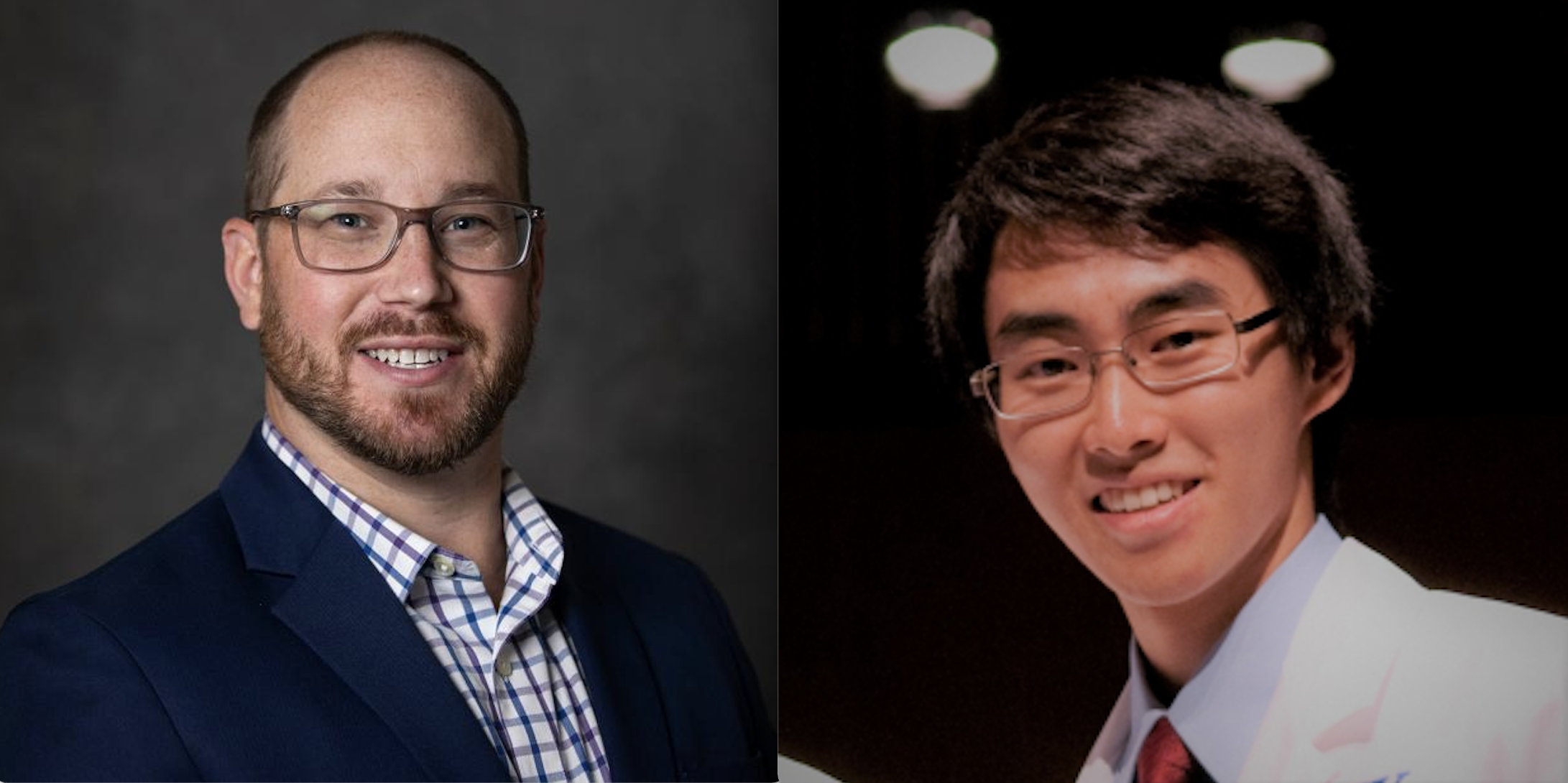
The two investigators are: Kirby Mayer, DPT, PhD and Yuan Wen, MD, PhD.
Mayer is studying muscle recovery after an Intensive Care Unit stay.
“We’re assessing long-term muscle, physical function recovery after something like an ICU stay for influenza COVID sepsis,” Mayer said. “People are fortunate to survive a stay in ICU. We’re studying what happens in that first year after recovery.”
The funding will allow Mayer time to refine his research, as well as study with mentors at Duke University and the Oklahoma Medical Research Foundation.
“We’d like to better understand why one patient can recover so quickly and get back to their life, while another can struggle with an arduous recovery, and maybe have complications, and have to go back to the hospital,” Mayer said.
It’s a topic that has been highlighted due to COVID, Mayer said, and this information could ultimately help healthcare workers provide better care.
“I think, uniquely, the College of Health Sciences positions us for these types of awards,” Mayer said. “Because of the interdisciplinary, inter-professional nature of the College, we’re able to collaborate with different departments. But we're also really positioned well to collaborate with other Colleges.
“That allows us to build that rich environment for research. We do have an interprofessional, interdisciplinary approach, and I think that's what really fosters good solid research in our College.”
Wen is studying a fine-tuning effect of protein synthesis in muscular dystrophy.
“There is a particular gene that is specific to the adult muscle,” he said. “It impacts how protein is made inside the tissue. Long story short, we found that this is changed with muscular dystrophy. Although most of this is a genetic disease that affects muscle protein, the loss of translation control is something that’s never really been looked at for this disease process, and it also opens up the potential that there is a wider impact on every other tissue as well.
“So, if we can switch out the components that makes protein, that means we can really fine-tune how protein is made more than we thought we were able to before.”
Muscular dystrophy is a debilitating disease, Wen said, but the mutations can vary from person to person.
“One of the things that we’re trying to understand is how come some people are so much worse off than others,” Wen said. “Is there anything we can do for them? Can we help improve their daily life, even if we can't cure them? They can't move. They can't breathe. Then, you know, once you can't breathe your heart stops pumping.
“In the worst cases these patients die really young, right?” he continued. “They barely make it to their twenties. These are really, severely sick patients.
“Even if we can't cure them completely, if we can help them maintain their ability to move during the first 20 years, I think that'll be pretty impactful, right?”
Wen also thanked the College, and especially the Center for Muscle Biology, for their support.
“There’s a lot of collaborative, supportive people and mentorship,” he said. “The more experienced people in the Center are very helpful in giving me advice. Everybody is willing to work together to contribute.”